Anterior cruciate ligament
The anterior cruciate ligament (ACL) provides stability and prevents anterior translation of the tibia. It originates from the medial aspect of the lateral femoral condyle and runs in an oblique fashion to insert into tibia. The ACL ruptures with pivoting when the foot is planted on the ground.
A pop is often felt and the injury is associated with pain, immediate swelling and blood in the knee. Treatment is still controversial and low demand patients and patients who are prepared to modify their lifestyles may be treated non surgical. Unfortunately latent instability can result in further injuries to the meniscus and articular cartilage causing early degeneration of the knee. When surgery is indicated the ACL nee

ds to be reconstructed with another graft tissue. The current graft options are the hamstring tendons and bone-patella tendon-bone graft. Quadriceps tendon and allograft (donor tissue) are other options.
Posterior cruciate ligament
The posterior cruciate ligament (PCL) stabilizes the knee and prevents posterior translation of the tibia.
Two different principle mechanisms have been described. High energy injuries occur with a direct blow to the tibia (dashboard injury). Low energy injuries can be non-contact with hyperflexion of the knee and the foot or occur with hyperextension of the knee. These injuries often occur with other injuries. Non-operative treatment with protected weight-bearing, rehabilitation and strengthening of the quadriceps muscle is indicated for low grade tears. If the PCL tears with a fragment of bone surgical repair results in good outcomes. PCL reconstruction is technically very demanding and is often less successful than ACL reconstruction. Residual laxity is not uncommon. In chronic injuries realignment of the tibia in both the frontal and lateral plane is useful and reduces the chronic posterior sag of the tibia.
Medial collateral ligament
The medial collateral ligament (MCL) is the most commonly injured ligament of the knee. It resists valgus (lateral bending). 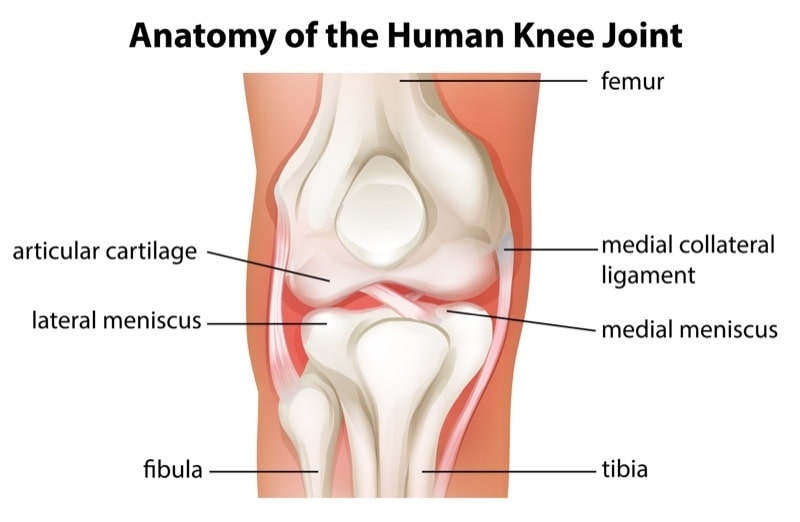 This is also the typical mechanism of injury. Tears usually occur at the femoral insertion. Mild sprains (grade 1) do not cause the fibers to tear with no loss of ligamentous integrity. Moderate sprains (grade 2) result in incomplete tearing and increase joint laxity. With severe tears (grade 3) there is complete disruption and gross laxity. Medial joint pain and difficulty walking due to pain or instability are signs of MCL injury. Grade 1 tears can be treated with pain killers, physical therapy and immediate weight-bearing. Return to normal activities can be expected at day 5-7. For grade 2 and 3 tears a hinged knee brace is normally indicated. With grade 2 the brace should be applied for 4 weeks and for grade 3 tears a minimum of 6 weeks is recommended. Most tears heal with brace treatment. However tibial tears have a lower potential to heal. Indications for surgery are rare. Surgery is indicated when multiple ligaments are torn (multi-ligament injuries, knee dislocation) and should be considered in professional soccer players.
This is also the typical mechanism of injury. Tears usually occur at the femoral insertion. Mild sprains (grade 1) do not cause the fibers to tear with no loss of ligamentous integrity. Moderate sprains (grade 2) result in incomplete tearing and increase joint laxity. With severe tears (grade 3) there is complete disruption and gross laxity. Medial joint pain and difficulty walking due to pain or instability are signs of MCL injury. Grade 1 tears can be treated with pain killers, physical therapy and immediate weight-bearing. Return to normal activities can be expected at day 5-7. For grade 2 and 3 tears a hinged knee brace is normally indicated. With grade 2 the brace should be applied for 4 weeks and for grade 3 tears a minimum of 6 weeks is recommended. Most tears heal with brace treatment. However tibial tears have a lower potential to heal. Indications for surgery are rare. Surgery is indicated when multiple ligaments are torn (multi-ligament injuries, knee dislocation) and should be considered in professional soccer players.
Lateral collateral ligament
The lateral collateral ligament (LCL) is more of a cordlike structure which runs from the femoral condyle to the fibula head. 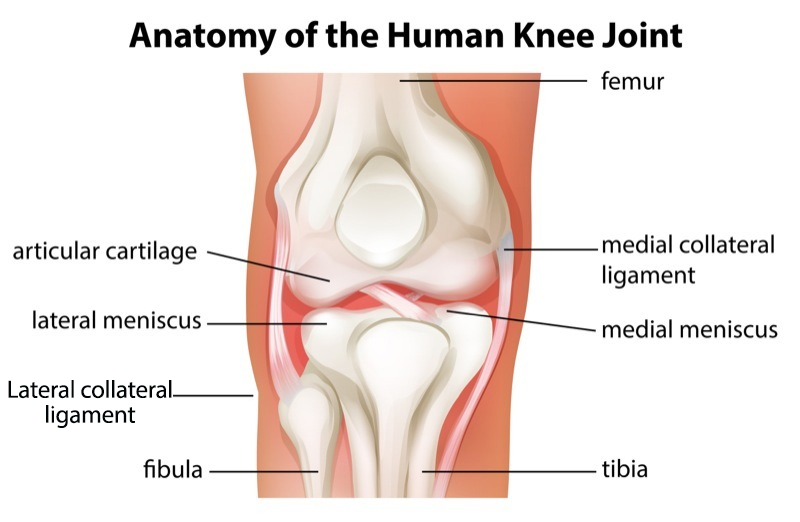 The primary function is to prevent varus (bowing). As it is located behind the flexion axis of the knee it is more tight in extension than in flexion. Similar to the MCL injuries can be graded into three types: grade 1 minimal tear, grade 2 partial tear and grade 3 complete tear. Injuries to the LCL are not common and are usually associated with other knee injuries. The most frequent mechanism is a direct blow to the weight-bearing knee or excessive varus force, external rotation of the tibia or knee hyperextension. Grade 1 and 2 injuries can often be treated with functional bracing and early rehabilitation. Acute repair should be considered in grade 3 injuries. In chronic injuries reconstruction is the better option. If the posterolateral corner is also ruptured surgical reconstruction is nearly almost indicated.
The primary function is to prevent varus (bowing). As it is located behind the flexion axis of the knee it is more tight in extension than in flexion. Similar to the MCL injuries can be graded into three types: grade 1 minimal tear, grade 2 partial tear and grade 3 complete tear. Injuries to the LCL are not common and are usually associated with other knee injuries. The most frequent mechanism is a direct blow to the weight-bearing knee or excessive varus force, external rotation of the tibia or knee hyperextension. Grade 1 and 2 injuries can often be treated with functional bracing and early rehabilitation. Acute repair should be considered in grade 3 injuries. In chronic injuries reconstruction is the better option. If the posterolateral corner is also ruptured surgical reconstruction is nearly almost indicated.
Posterolateral collateral corner
The posterolateral corner (PLC) contains multiple structures. Static stabilizers are the popliteus tendon, popliteofibular ligament, the lateral knee capsule and the arcuate ligament.  Dynamic stabilizers include the biceps femoris muscle and tendon, the popliteus muscle, the iliotibial tract and the lateral head of the gastrocnemius muscle . The controls external rotation, varus and posterior translation. The PLC is injured with blows to the antero-medial aspect of the knee, a varus blow to the flexed knee, contact and non-contact hyperextension injury and knee dislocations. Injuries to the common peritoneal nerve occur in 15-30% and result in a dropped foot.
Dynamic stabilizers include the biceps femoris muscle and tendon, the popliteus muscle, the iliotibial tract and the lateral head of the gastrocnemius muscle . The controls external rotation, varus and posterior translation. The PLC is injured with blows to the antero-medial aspect of the knee, a varus blow to the flexed knee, contact and non-contact hyperextension injury and knee dislocations. Injuries to the common peritoneal nerve occur in 15-30% and result in a dropped foot. 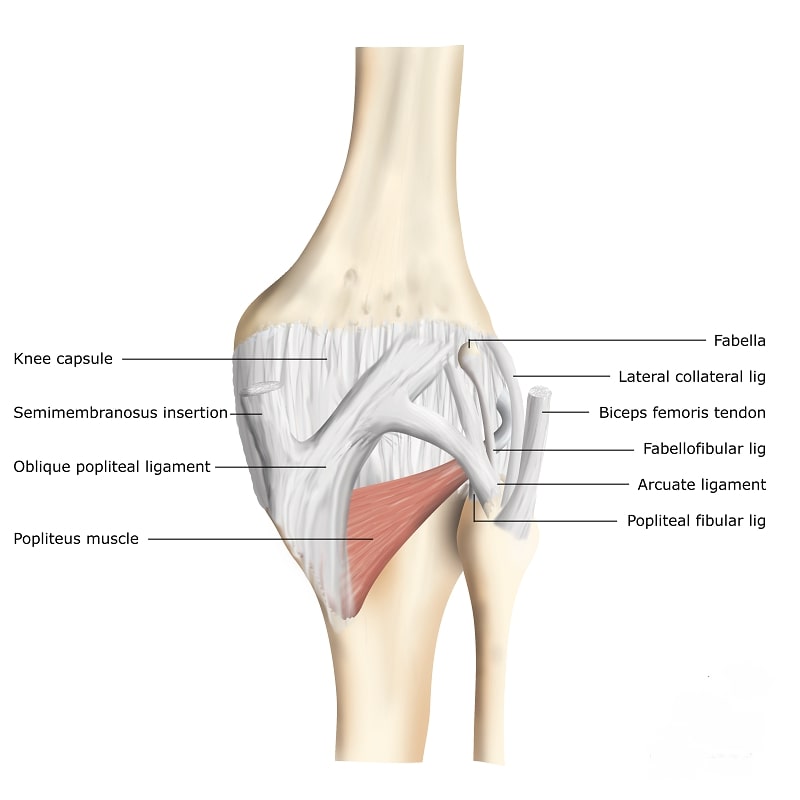 Patients often have the feeling of instability when the knee is in full extension or have trouble climbing stairs, pivoting and cutting. Isolated PLC injuries are rare and if only grade 1 or 2 can be treated with protected weight-bearing in full knee extension followed by progressive functional rehabilitation. Grade 3 injuries require surgical reconstruction/repair. Similar to chronic PCL injuries the leg should be realigned in both the frontal and lateral plane. In general reconstructions are preferred over repair as they have a lower revision and failure rate.
Patients often have the feeling of instability when the knee is in full extension or have trouble climbing stairs, pivoting and cutting. Isolated PLC injuries are rare and if only grade 1 or 2 can be treated with protected weight-bearing in full knee extension followed by progressive functional rehabilitation. Grade 3 injuries require surgical reconstruction/repair. Similar to chronic PCL injuries the leg should be realigned in both the frontal and lateral plane. In general reconstructions are preferred over repair as they have a lower revision and failure rate.
Posteromedial corner
The posteromedial corner (PMC) is comprised of five major components. 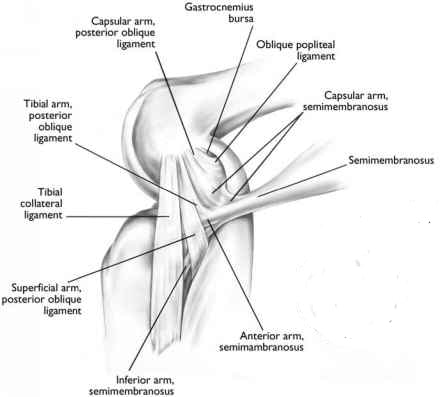 They are called the posterior oblique ligament, the semimembranosus tendon with its expansions, the oblique popliteal ligament, the posteromedial joint capsule and the posterior horn of the meniscus. The mechanism of injury is either a valgus force most commonly occurring during athletic activity or anteromedial rotation of the knee. They are commonly observed with associated knee injuries in particular combined ACL and MCL ruptures. The posterior oblique ligament (POL) is the most commonly injured structure. Non-operative treatment is indicated in low grade medial knee injuries that involve both the MCL and PMC. The treatment protocol for MCL injury is usually followed. Multi-ligament injuries, knee dislocations, avulsions of both the MCL and PMC and chronic injuries with antero-medial rotation instability are indications for surgery.
They are called the posterior oblique ligament, the semimembranosus tendon with its expansions, the oblique popliteal ligament, the posteromedial joint capsule and the posterior horn of the meniscus. The mechanism of injury is either a valgus force most commonly occurring during athletic activity or anteromedial rotation of the knee. They are commonly observed with associated knee injuries in particular combined ACL and MCL ruptures. The posterior oblique ligament (POL) is the most commonly injured structure. Non-operative treatment is indicated in low grade medial knee injuries that involve both the MCL and PMC. The treatment protocol for MCL injury is usually followed. Multi-ligament injuries, knee dislocations, avulsions of both the MCL and PMC and chronic injuries with antero-medial rotation instability are indications for surgery.
